Long Haulers: Symptoms, Treatments & Understanding After Effects of COVID
It is almost impossible not to think about the COVID-19 pandemic on a daily basis - you may have symptoms, your family is getting tested, your friends or coworkers have COVID, you get updates on your phone, you watch coverage of the pandemic on television.
You’ve surely heard about long-haul COVID. Or, perhaps one of the other terms used to describe the same thing (or the person with long-haul COVID): long-hauler/long-haulers, long COVID, chronic COVID, long-hauler COVID, post-acute COVID-19, post-COVID syndrome, late sequelae of SARS-CoV-2, etc.
Worldwide research on COVID-19 and long-haul COVID is ongoing. There is a constant flow of new data and information about prevention, symptoms, diagnosis, and treatment. Doctors and researchers are using results from these studies to develop ways to care for their COVID patients.
The information about COVID-19, and now long-haul COVID, can be overwhelming and confusing. And it changes - often every day. What follows is an overview of long-haul COVID. It will provide answers, based on the data and information we have today to the question: What is long-haul COVID?
Here's what we'll cover:
What is Long-haul COVID?
(name=whatscovid)Long-haul COVID follows an initial COVID infection caused by the coronavirus, or SARS-CoV-2.
There are various descriptions of long-haul COVID. The Centers for Disease Control and Prevention (CDC) describes long-haul COVID as follows:
“Some patients who have been infected with SARS-CoV-2, the virus that causes COVID-19, have new, recurring, or ongoing symptoms and clinical findings four or more weeks after infection, sometimes after initial symptom recovery.”
People with long-haul COVID have signs and symptoms at least 4 weeks after their initial infection. These signs and symptoms:
Are new and different, OR
Return after going away, OR
Never went away and continue
What Does Initial COVID Infection Mean?
(name=infection)Initial infection is part of the description of long-haul COVID, but what does it mean? It actually has several different meanings as follows:
You have COVID symptoms that may be very mild, moderate, or severe OR;
You have an initial infection, do not have COVID symptoms (you are asymptomatic) AND one of the following:
Positive test results
False-negative test results (you have the virus, but test results don’t show it)
No test results
You can have long COVID with or without symptoms during initial infection and with or without clear test results or any testing at all.
What Does COVID Infection Do to the Body?
(name=covidbody)Although we don’t fully understand what coronavirus does to the body, it has the ability to invade many types of cells. Extreme inflammation, immune system damage, brain-nerve communication dysfunction, increased blood clot formation, etc. may occur.
What results from the coronavirus’ invasion of cells, tissue, and organs? A wide range of possibilities from minimal to minor symptoms, but also severe, acute COVID; and long-haul COVID.
Severe, Acute COVID
People with severe, acute COVID are very ill. They may have long hospitalizations, usually in intensive care units (ICU). They often require life-saving treatments, like intubation and mechanical ventilation. Those who survive may have serious long-term effects.
The virus may damage the cells of your heart, blood vessels, lungs, brain, nerves, kidneys, and other organs.
A person may have serious, life-threatening complications like heart muscle (myocardial) damage, irregular heart rhythms (arrhythmias), scarred lungs (pulmonary fibrosis), seizures, or stroke.
The longer hospital stays and the treatment may have additional long-term consequences. There is even an illness called post-(ICU) intensive care unit syndrome (PICS). Despite its name, post-ICU care syndrome is associated with longer hospitalizations overall.
Hospitalization-related effects may include generalized weakness, difficulty with thinking skills and memory, emotional issues, and long-term disability.
Long-haul COVID
Long-haul COVID may occur following initial COVID infection. But just as initial COVID infection differs from person-to-person, so does long-haul COVID.
How Common is Long-Haul COVID?
(name=common)Long-haul COVID is common, although studies of the number of people vary. One study found 1 out of 3 people had symptoms up to nine months after acute COVID infection. Other analyses determined even higher numbers.
What are the Risk Factors for Long-Haul COVID?
(name=risk)Study results are conflicting - meaning some find certain factors increase the risk of long COVID, while others find those same factors do not increase the risk. Some of the risk factors may be:
Being female
Having more than five symptoms during acute COVID
Developing severe acute COVID (Severity does increase the risk of long COVID, but it can occur in someone with or without severe acute COVID)
Having three or more existing chronic medical conditions
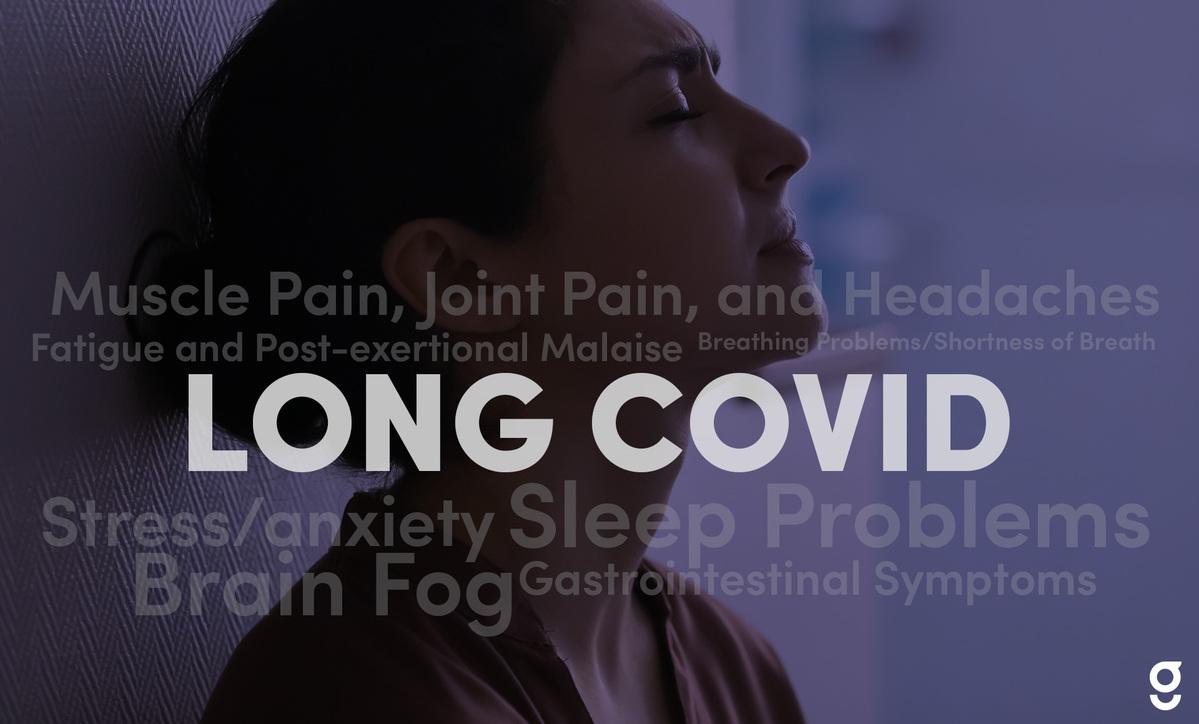
What are the Symptoms of Long-Haul COVID?
(name=symptoms)The symptoms of long-haul COVID are different from person-to-person (i.e. fatigue vs. loss of taste/smell, etc.). The length of time (weeks to months) and the number of symptoms present (one to many) also varies.
There are dozens of symptoms in people with long-haul COVID. According to some research, fatigue, post-exertional malaise - PEM (extreme fatigue even after minor physical or mental tasks), and brain fog (trouble with thinking, concentration) are the most common ones. Several others are loss of taste and smell, headaches, brain fog, trouble sleeping, muscle and joint pain, and difficulty breathing/shortness of breath.
What is the Treatment for Long-Haul COVID?
(name=treatment)There is no cure for long COVID. Every day, doctors and researchers are figuring out the best treatments for long-haul COVID symptoms. They use treatments backed by scientific evidence that show they are safe and that they work. Doctors and other experts have:
Learned and shared data and information from their own COVID-19 cases
Established long COVID treatment centers or clinics throughout the U.S.
Used treatments for other conditions with similar symptoms. For example, to treat fatigue they’ve looked at chronic conditions like chronic fatigue syndrome (CFS)/myalgic encephalomyelitis (ME), rheumatoid arthritis (RA), and multiple sclerosis (MS)
Created treatment guidelines. As an example, the American Academy of Physical Medicine and Rehabilitation (AAPMR) has treatment guidelines for long COVID fatigue, breathing discomfort, and cognitive symptoms (e.g. brain fog)
Treatments for Common Symptoms of Long-Haul COVID
Available treatments for long-haul COVID depend on your symptoms. These treatments can help lessen symptoms while giving your body time to heal. Some treatments are available to you through Goodpath’s long COVID program. However, there are some that only your doctor or a specialist can provide.
Some long-haul COVID symptoms may also be treated by Goodpath and your doctor together. For example, Goodpath may provide treatments for sleep problems (e.g. nutritional supplements, cognitive behavioral therapy for insomnia [CBT-I]), while others require your doctor (e.g. prescription sleep medications).
Symptom-Specific Treatments
Fatigue and Post-exertional Malaise (PEM)
It takes time and patience to cope with fatigue and PEM. Treatment may include a healthy diet, e.g. anti-inflammatory foods, staying well-hydrated, slowly returning to activities, and daily activity planning (e.g. taking time to rest throughout the day). Our Goodpath coaches can help.
Treating other problems like trouble sleeping, depression, or anxiety is also important.
Brain Fog
Treatment focuses on managing brain fog since there isn’t a cure. It may also include a healthy diet like the Mediterranean diet, staying well-hydrated, and exercise/physical activity. Cognitive support techniques and mind/body exercises help people with brain fog.
Support from family and friends is important. Our Goodpath coaches also offer support and help with diet, etc.
Treating other problems like trouble sleeping, depression, or anxiety may also be part of the treatment. Your doctor may check all of your medicines for side effects that can worsen brain fog.
Sleep Problems
Sleep problems are common in long-haul COVID. They may also worsen other symptoms. Treatment may include nutritional supplements, mind-body exercises (e.g. meditation, journaling, and yoga).
It may also incorporate Cognitive Behavioral Therapy for Insomnia (CBT-I) and sleep hygiene (e.g. amount of sleep, diet, caffeine, etc.).
Addressing other problems like depression or anxiety may be included. Your doctor may also recommend prescription medication.
Muscle Pain, Joint Pain, and Headaches
Painful conditions may occur with long-haul COVID. Treatment may include muscle/joint-specific exercises and physical activity, a healthy diet (e.g. anti-inflammatory foods) or mind-body exercises, such as meditation, journaling, or yoga.
It may also include nutritional supplements, OTC medicines (e.g. pain relievers, creams, gels, etc.), heat therapy, and addressing other problems (e.g. trouble sleeping, depression, or anxiety). Your doctor may also recommend prescription medication.
Breathing Problems/Shortness of Breath
Treatment may include breathing exercises (e.g. pursed-lip breathing) or use of a breathing device (spirometer), positioning to aid breathing, exercise and physical activity, a healthy diet (e.g. anti-inflammatory foods) and smoking cessation.
Your doctor may recommend prescription medication, oxygen, rehabilitation programs, or referral to a specialist (pulmonologist).
Stress/anxiety
Many people with long-haul COVID have increased anxiety and stress. Treatment may include a healthy diet (e.g. anti-inflammatory foods) nutritional supplements, mind-body exercises (e.g. breathing techniques, meditation, journaling, or yoga), support from friends and family, counseling, or prescription medications from a doctor.
It’s also important to address other problems like trouble sleeping and depression.
Gastrointestinal Symptoms (e.g. nausea, diarrhea, etc.)
GI symptoms like nausea, diarrhea, etc. may be present. Treatment may include healthy eating (e.g. anti-inflammatory foods) nutritional supplements, OTC medicines, and mind-body exercises (e.g. meditation, journaling, yoga). Your doctor may recommend prescription medications in some cases.
Can Long-Haul COVID be Prevented?
(name=prevention)Once you have an initial COVID infection, whether or not you have symptoms, there isn’t a treatment to prevent long-haul COVID from developing. The better questions may be: Can the initial COVID infection be prevented? Can severe, acute COVID be prevented?
Preventing Initial COVID-19 Infection
As you know, there are things you can do to prevent COVID-19 infection that greatly reduce the risk of severe, acute COVID.
This includes:
Information. Be cautious of sources. Double-check facts. Watch for new information as study data becomes available.
Vaccinations. Be sure to get all doses and boosters.
Masks. Wear the safest mask available.
Socially distancing. Stay at least 6 feet apart from others.
Avoiding crowds. Know who you’re around.
Isolate. When sick or exposed, isolate and get tested.
Basics. Wash your hands. Cover your mouth and nose when coughing or sneezing.
Preventing Severe, Acute COVID-19
The following are out-of-hospital treatments for preventing severe, acute COVID.
Oral Antivirals
A course of antiviral medication may be prescribed for some people with COVID-19 infection. Antivirals help to reduce the risk of hospitalization and death in certain individuals who are likely to have severe, acute COVID.
Monoclonal Antibodies
Monoclonal antibody therapy is available for adults and children at least 12 years old who have an increased risk of severe, acute COVID. It may be administered to those who have positive test results and symptoms within 10 days of symptom onset.
When Should You See Your Doctor for long-haul COVID Symptoms?
(name=doctor)If you have any of the following symptoms you should see your doctor or get medical care:
Breathlessness at rest
Chest pain or tightness
Fever
Muscle or joint pain with loss of sensation, numbness, changes in skin color, swelling, or pain spreading to other areas of the body
Does an Integrative Approach Work for long-haul COVID?
(name=integrative)Yes, an integrative approach can work very well because it uses the best of conventional and complementary medicine. It puts the person at the center of care and addresses all of their needs (e.g. physical, emotional, cognitive, etc.). In fact, CDC guidance for optimizing Long COVID care recommends a whole-person approach including exercise therapy, activity pacing, cognitive support, OTC medicines, and lifestyle changes for underlying conditions.
Goodpath and Long-haul COVID
Goodpath provides a program for people with long COVID. We use an integrative approach that includes specific exercises and activity guidance, mind-body techniques, nutritional supplements, OTC medicines, and diet support. Take our assessment to get started.